COVID-19: Making sense of the statistics
Struggling to make sense of the numbers surrounding COVID-19? You're not alone. Dr. Jason Salemi, an epidemiologist and data expert at USF's College of Public Health shares his analysis to help health providers, public policymakers, parents, teachers, and others make wise decisions.
Amidst the constant media updates on the pandemic, it’s easy to become bewildered by its myriad of statistics.
Knowing someone affected by COVID-19 profoundly impacts our feelings about the scourge, but making sense of the constant barrage of numbers can help our understanding of it.
With that in mind, 83 Degrees asked Dr. Bruce Shephard of Tampa to interview Dr. Jason Salemi, a local epidemiology and data expert from USF. Dr. Salemi is an Associate Professor of Epidemiology at USF’s College of Public Health, with over 150 scientific publications and expertise in visualizing and analyzing data. His comprehensive dashboard tracking COVID-19 in Florida has received national attention as a guide to better understand this disease.
Here are five takeaways Dr. Shephard compiled from his conversation with Dr. Salemi.
1. All reporting sources are not equal — and certainly not standardized
For starters, Dr. Salemi notes “when we talk about COVID-19 data metrics, a lot of issues emerge from the fact that there are no comprehensive national standards at present.” As an example, he points out “the CDC has not come out and said ‘this is a benchmark measure or series of benchmark measures for returning to schools in person’ or something even simpler like ‘this is how we recommend that states measure and report on something like the case positivity rate’.“
Federal and state-based reporting do not align all that well for some measures. In Florida and all other states, current COVID hospitalizations are reported by both the state — in Florida, that’s the Agency for Health Care Administration (AHCA) – and from the federal Department of Health and Human Services (HHS). Those two sources may derive quite different results, according to Dr. Salemi, because states each use their own criteria to document current hospitalization rates; often this is different from the federal definition.
In Florida, the state only reports COVID admissions if COVID is documented as the primary diagnosis for hospitalization, whereas federal reporting includes all hospitalizations for patients “who have suspected or confirmed COVID-19.” It also appears as though part of the difference may be attributed to facilities included in the report. The feds appear to include VA hospital and state correctional admissions whereas AHCA does not cover those state and federal hospitals. On balance, these reports give a slightly lower hospitalization rate for COVID patients in Florida’s state-based accounting.
For example, on 8/18/20 the state listed 5,610 admissions compared to the HHS listing of 7,171 on the same day, a 22% difference. Fed/State reporting variances result in relatively small differences in some states, notes Dr. Salemi, “but it can sometimes be considerable as in Arkansas and Nevada, which in the past few weeks have seen state-reported COVID admission rates three times lower compared to HHS’ numbers.”
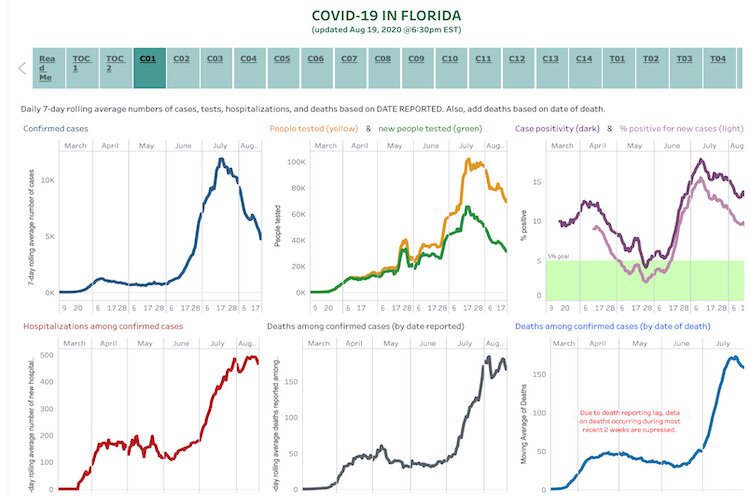
Ever the epidemiologist-sleuth, Dr. Salemi closely follows these and other official daily reports on his COVID Dashboard, which is available to the public on his website. He also frequently tweets out important updates (@JasonSalemi) and has a YouTube channel that tries to add clarity to some of these dense topics.
2. Each statistical measure has a unique level of significance
Dr. Salemi avoids dwelling upon any single statistic to define the pandemic. His approach is that each metric derives its significance depending on context, upon what question or decision one is trying to answer.
“For example, if looking into the recent spread of severe disease, current COVID-19 hospitalizations and deaths would be the primary focus,” he explains. Now with Florida transitioning out of near lockdown and many schools about to reopen, he believes there are two specific metrics that academicians have tended to “pay attention to” and which stakeholders must now examine closely in deciding how and when to open schools safely.
These are “case positivity rates” and “degree of recent community spread of the virus.” With “case positivity rates” Florida reports and calculates this metric in two separate ways, making the process of incorporating these measures into decision making a bit confusing.
3. Florida reports “case positivity rates” for COVID-19 in two ways — with somewhat different results
Florida calculates COVID case positivity rates on both a daily and a weekly basis but reports two different measures to define it. The first measure, call it simply “case positivity,” takes the number of individuals who test positive and divides it by the total number of individuals tested that day. Simple enough. A second measure, the “percent positivity for new cases,” is done just like the first except that it excludes people who tested positive on any previous day.
The net effect of this second measure in practice is to derive a lower percentage than the first measure (case positivity) — by around 3-4% in recent weeks — and it is this metric that the state tends to use for county-level estimates, according to Dr. Salemi. Also, he emphasizes, the difference between the two positivity measures is magnified by repeat testing, which is exactly the situation we now have in Florida, where currently 50% of people being tested each day are not being tested for the first time; they are repeating their tests. As of this writing, during the past 7 days, Florida’s average case positivity rate (the first method) was almost 13% while the rate using the second calculation was 9%.
The point, Dr. Salemi stresses, is that “while both methods trend similarly, the problem comes in if we’re trying to establish a benchmark goal, which, in the case of school reopenings, should be at 5% or less case positivity, according to many experts.
Here, which calculation method is used assumes great significance and the public must now digest both measures and their different results to make informed decisions around public health policy.”
For last week, Hillsborough County reported a positivity rate (using the “percent positivity for new cases”) of 7.9% and Pinellas County reported a rate of 4.9%. Dr. Salemi also stressed that “an argument can be made for using each measure, but no formal recommendations have been made from the government.”
4. Community spread is a metric in which geographic variation complicates health messaging
The other factor epidemiologists consider essential in regard to school openings is recent “community spread.” This metric is defined as the number of new cases per day per 100,000 people, usually focusing on just the last 7 or 14 days. To date, general agreement about what number constitutes a safe benchmark for “community spread” has not been established among experts, let alone the CDC.
A few cases per day/100,000 is a lofty ideal, according to Dr. Salemi, but other academicians and experts have also suggested a range of 10-25 cases/d/100,000 as at least an initial goal.
As of this writing, Florida reports in the past 7 days, a community spread of 29 cases/d/100,000 but the countywide variance is huge, ranging from a low in Martin County (10 cases/d/100,000) to the highest currently in Lafayette County (1,377 cases/d/100,000), where the alarmingly high rate must be put in context since it is mostly due to high COVID spread in a correctional facility in that county.
Hillsborough County reported community spread of 17.2 and Pinellas County 13.4 in the past week, pretty much within the broad guidelines that have been recommended prior to school reopening.
5. Transparent statistical reporting is key to effective public policy
Our understanding of COVID-19’s biology — a moving target — has contributed to some confused messaging around the statistics that seek to explain it. However, complex virology aside, the absence of a coherent state-based or federal public policy has made Florida’s response to the pandemic all the more difficult.
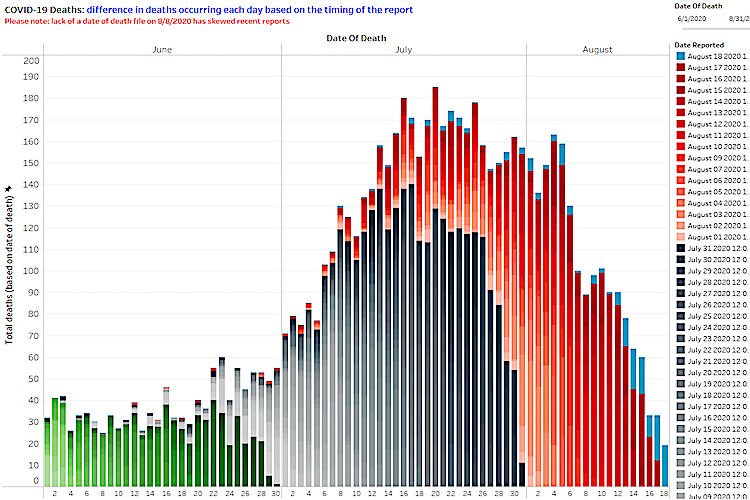
That said, Dr. Salemi reports he’s an optimist, saying “trends in the current measures to which I have access are looking good” when he goes into his dashboard, which reflects decreases in COVID-19 cases per day, in case positivity numbers, and in the number of people currently hospitalized with COVID-19, since mid-July.
The lower case counts are at least in part being driven by decreasing numbers of new people who are tested daily, but he is hopeful the decrease reflects mostly the public’s increasing adherence to mitigation measures like masks and social distancing.
As far as schools reopening, Dr. Salemi says that schools are rightfully being asked to do a lot to prevent spread of the virus to students, teachers, and staff.
Among these mitigation efforts, he stresses the critical importance of two factors which, if managed appropriately, are likely to minimize COVID spread: reduced class size with greater spacing (so-called ‘de-densifying’) and the universal use of masks.
Beyond broader statistical guidelines, Dr. Salemi stresses families will and must make their own very personal decisions and consider their unique circumstances including medical conditions and proximity of older family members in addressing issues such as returning to brick-and-mortar schools.
Looking ahead, he notes, further research must address a better understanding of asymptomatic transmission in children.
“How does it occur? Are children as infectious as adults? What are the long-term effects?” he asks. “We also need to determine which mitigation strategies are most effective – ventilation, masks, hygiene – to inform policy decisions about pediatric health and school openings,” he adds.
With Tampa schools planning to open up this month, hopefully, all stakeholders involved will take advantage of a growing understanding of the statistics behind this pandemic. Perhaps Dr. Salemi’s dashboard and his efforts with the national Coronavirus in Kids (COVKID) Tracking and Education Project will help.
Dr. Jason Salemi is an Associate Professor at the University of South Florida College of Public Health and Morsani College of Medicine in Tampa.
Bruce Shephard is a retired Tampa Obstetrician-Gynecologist and Affiliate Associate Professor, Department of Obstetrics and Gynecology, USF, Morsani College of Medicine.
Epidemiologist Dr. Jason Salemi of USF shares Florida data in CNN interview.